Introduction:
For the COVID-19 (SARS-CoV-2) response, rapid diagnostic tests (RDTs) for COVID-19 antigen (Ag) and antibody (Ab) are expected to complement core molecular tests, particularly in low-resource settings. This review assesses the requirements for the implementation of the COVID-19 PDRs in Sub-Saharan Africa.
Methods:
Review of articles published in PubMed evaluating COVID-19 PDRs supplemented with product instructions for use (IFU).
Results:
In total, 47 articles were retrieved on two COVID-19 Ag PDRs and 54 COVID-19 Ab PDRs and IFUs of 20 COVID-19 Ab PDRs. Only five COVID-19 Ab PDRs (9.3%) were evaluated with capillary blood samples at the point of care; none of the studies was conducted in sub-Saharan Africa.
- Sampling: Challenges for COVID-19 Ag PDRs include nasopharyngeal sampling (technique, biosafety) and sample stability; For COVID-19 Ab PDR, the equivalence of whole blood vs. plasma/serum needs further validation (evaluated for only eight (14.8%) products).
- Specificity: The sensitivity of the COVID-19 Ag and Ab PDRs depends on the viral load (antigen) and the time period (antibody), respectively; COVID-19 Ab tests have a lower sensitivity compared to laboratory test platforms and the kinetics of IgM and IgG are very similar. Reported specificity was high, but has not yet been evaluated against tropical pathogens.
- Kit setup: For COVID-19 Ag PDRs, flocked swabs should be added to the kit; for COVID-19 Ab PDRs, fingerstick sampling materials, transfer devices, and controls must be added (currently only supplied on 15, 5, and 1/20 products). Ease of use and robustness: Some Ab PDRs for COVID-19 showed high proportions of faint lines (> 40%) or invalid results (> 20%). Deficiencies were reported in the buffer vials (spillage, air bubbles) and their instructions for use.
- Stability: the storage temperature was ≤ 30 ° C for all but one RDT, the stability in use and results was maximum at 1 h and 30 min, respectively. Integration into the healthcare environment requires a targeted product profile, an overview of the technology landscape, certified manufacturing capacity, a sustainable marketplace, and strict but timely regulation. Deployment in the country depends on integration into the national laboratory network.
Discussion / Conclusion:
Despite these limitations, successful implementation models have been proposed in triage, contact tracing, and surveillance, particularly for COVID-19 Ab PDRs. There is valuable experience from the implementation of other disease-specific RDPs in sub-Saharan Africa.
Antigens and Molecular Tests for COVID-19
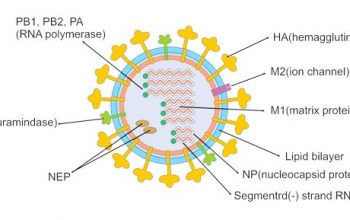
The field of diagnostic testing for COVID-19 is rapidly evolving, with many tests focused on diagnosing patients with active viral infections. Diagnostics capable of detecting current active infections are usually antigen- and molecule-based tests. These tests inform researchers and healthcare providers of the presence of the pathogen, either by amplifying and detecting its genetic material or by identifying unique markers for the pathogen itself. The viral genomic material for SARS-CoV-2 is ribonucleic acid (RNA), which remains in the body only while the virus is still replicating, even at very low levels.
Antigen tests detect specific viral proteins (antigens) present in a patient sample taken with nasal or nasopharyngeal swabs and can provide results in less than half an hour. Antigens are found on the surface of the virus particle, which is also shed in the patient’s tissues. These rapid tests detect the baseline antigen levels that are already present in a sample, providing only a simple “yes” or “no”, similar to a pregnancy test.
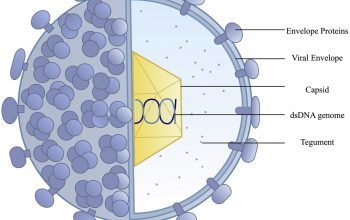
Molecular tests called nucleic acid amplification tests (NAATs) are based on the amplification of the genetic material in the sample. NAATs include the polymerase chain reaction (PCR) assay in a laboratory to amplify viral genomic material for detection and can provide results within hours or days; other techniques include LAMP and next-generation sequencing. These tests require samples from the patient that is likely to contain viruses. Most samples are collected using nasopharyngeal swabs or a sputum cup, although the virus can also be detected in stool, urine, or blood.
For illnesses that are primarily respiratory in nature, such as COVID-19, nasopharyngeal swabs have been the most reliable, taking samples from an area of the respiratory tract where the virus appears to first infect an individual. This site is relatively easy to access, compared to the final site of viral infection: the lower respiratory tract. The nasopharyngeal tract is likely to have (1) active virus replication and (2) enough virus to be detected in test kits.
Note on sensitivity and specificity data
Where available, we list manufacturer-reported sensitivity and specificity data. A highly sensitive test should capture all true positive results. A highly specific test should rule out all true negative results. These measures are not independently validated by the Johns Hopkins Center for Health Safety. If sensitivity or specificity is not listed, the manufacturer did not provide it at the time of publication. When available, the number of samples used for sensitivity/specificity definitions are listed in the product description.
The terms “sensitivity” and “specificity” may not appear on manufacturers’ information sheets, but are often reported as “positive per cent agreement” and “negative per cent agreement.” Sensitivity can also be measured by calculating the limit of detection, which is the lowest detectable number of virus copies in a sample where the test will be positive at least 95% of the time. Essentially, a lower limit of detection indicates a more sensitive test, with fewer viral copies per sample required to obtain a positive test result.